Sending Medicare Secondary Claims with the Validator 6 and 5010
Background:
Validator 6 was designed specifically to address the issue of sending PRIMARY insurance claims to any carrier who accepts a HIPAA compliant form file. That being said, there is often a need to also send secondary claims electronically through the Validator 6, especially to Medicare.
There are, however, some limitations to the Validator 6’s ability to send these secondary claims. Specifically, the practice management systems which we support simply DO NOT contain the fields necessary to get claims paid when sent as a secondary. This coordination of benefits information simply is not available in any of the Lytec programs, and to be fair, most practice management systems are not designed to carry this information like they should be.
While this is likely a future enhancement you will see in all practice management systems, we have a need NOW to send claims in this manner, as many Medicare intermediaries are either strongly compelling or outright forcing providers to submit their secondary claims electronically.
Thus we have made sure with our Validator 6 that our clients have the ability to send these claims electronically, with the use of Lytec’s ability to use custom fields to provide the missing information. These changes reflect the current 5010 changes and have been tested with the Medicare system.
What you will need:
The changes neccesary to make Validator 6 able to send the extra fields Medicare has been asking for make it neccesary for you to have the following in order to be able to send it:
- Validator 6 version 6.0.5.0 or greater. If you do not have it, visit our downloads page to find the latest update, or use the auto updater feature in the Validator 6 software.
- One of the following form files, or a newer revision (the revision is the number after the “r” or “rev” in the file name, so the 2011 form below is revision 4. Any revision above 4 will work). These files are available on our downloads page or you can get them directly from your Validator 6 reseller. If you do not see these when you go to billing\print insurance claims, you go to your Validator 6 and choose settings\carrier setup options and click on the form files tab. Find the form you need and press the “Refresh Form Files” button.
- _Eclaims 5010 for Lytec 2011_r4.lns
- Lytec 2011. The older versions (2010 and older) do not have the custom fields neccesary to send Coordination of Benefits information at the CPT level. These previous versions are also not 5010 compliant due to missing fields in the program.
- You will also want to, as a matter of course, have the latest service pack for your Lytec program installed, many of which are provided for your convenience on our downloads page.
Setting Up Lytec
The following fields are required now in order to get your secondary claims paid.
Patient Level Information
• Medicare Secondary Payer Type
CLAIM LEVEL COB INFORMATION
• Coordination of Benefits (COB) Payer Paid Amount
• Coordination of Benefits (COB) Allowed Amount
• Claim Adjudication Date
SERVICE LINE COB INFORMATION
• Coordination of Benefits (COB) Primary Payer Line Item Approved (aka Allowed) Amount (AMT02)
• Coordination of Benefits (COB) Primary Payer Line Item Paid Amount (SVD02)
• Coordination of Benefits (COB) Primary Payer Line Item Adjustment Amount (CAS03)
• Coordination of Benefits (COB) Line Item Expected Amount (usually this is the Patient Responsibility Portion)
Note that we should re-iterate that there are many pieces of information that are required at the detail level. This means that we have to utilize the billing detail custom fields which are available only on Lytec XE or newer versions. If you have the need to send Medicare Secondary Claims electronically, and are still on Lytec 2001 or prior, we highly encourage you to upgrade your Lytec system.
PREPARING FOR MEDICARE SECONDARY CLAIMS
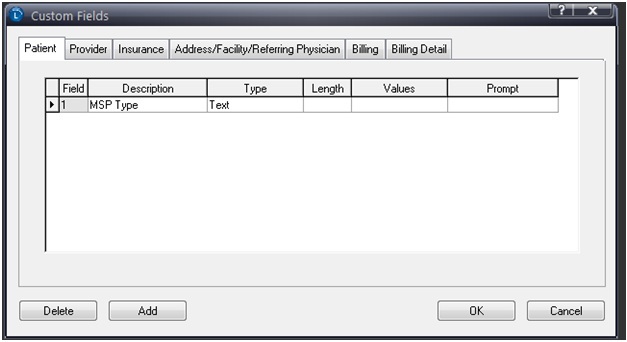
You will need to set up custom fields to hold the information Medicare is now requiring. To do this, go to Settings\Custom fields from within your Lytec program.
Click on the Patient tab and fill in the fields as shown below:
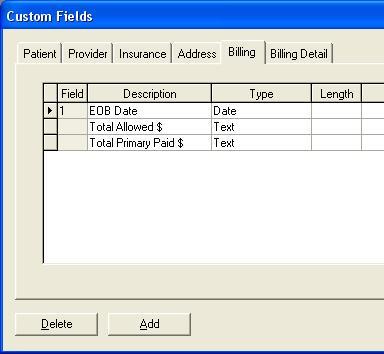
Click on the Billing tab and fill in the fields as shown below:
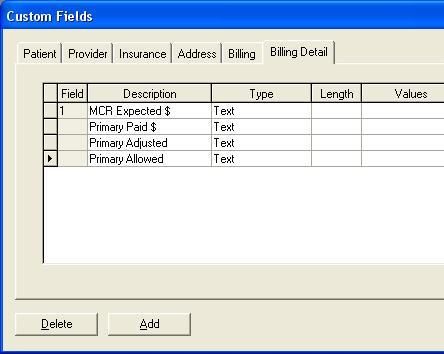
Then click on the Billing Detail tab and fill in the information as follows:
Now before sending your Secondary Medicare claims off, you will need to fill in Coordination of benefits information on the charges and payments screen. Click on Billing\Custom fields to fill in (in this order):
1. The EOB Date
2. The total claim allowed amount
3. The total claim adjusted amount
Then go to each detail line, click on Detail\Custom Fields to fill in (in this order):
1. How Much You expect Medicare to Pay for this procedure (usually the patient responsibility portion)
2. The Primary Insurance Paid Amount for this procedure
3. The Primary Insurance adjusted amount for this procedure
4. The Primary Insurance Allowed amount for this procedure
When filling in the custom fields, you should consider the following:
1. The Line Item Date of Adjudication is Taken from the Claim Adjudication Date
2. If Claim Detail – Custom Field 3 is not filled in, we will not pull any information from custom fields 4 and 5 (no adjustment information)
3. All Date custom Fields must be set as a Date field in Lytec
6. All Amount fields must be entered with the smallest number of characters necessary. For Example, $50.00 would be just 50, $50.50 would be 50.5 and $50.23 would be 50.23.
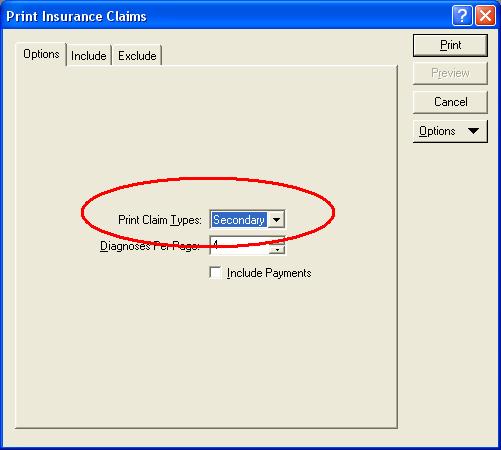
Finally, when printing the claims, you will need to remember to make sure to choose types of Claims as “Secondary”